Advances in cancera disease where abnormal cells split without control and spread to other nearby body tissue and/or organs care have evolved this decade more rapidly than ever before. The main contributor to this is the advent of precision medicine. The Human Genome Project has altered the cancer research trajectory, demonstrating that the original ‘one-size-fits-all’ approach to treatment requires updating to a more individual approach of approaching each cancer according to its unique characteristics and not where the primary site is.
Where once there were only three main conventional modalities, now there are numerous emerging therapies – often used in combination for optimal outcomes; all with marked increases in efficacy and patient survival.
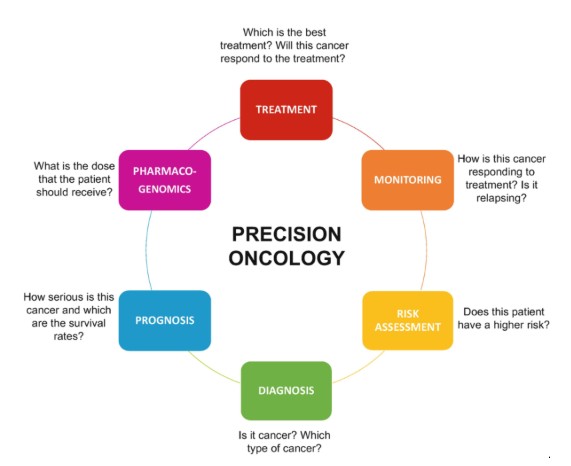
But first, let’s explain what Next Generation Sequencing (NGS) means. NGS uses genome testing (see previous article about genome testing) to identify faulty, cancer-causing gene mutations. It has fundamentally changed the scientific world because it enables scientists to sequence millions of DNA molecules simultaneously, allowing detection of new targets for both diagnostic tests and cancer treatments. This is called precision oncologythe study, diagnosis and treatment of cancer – where a treatment plan can be tailored according to the specific cancer mutation, not according to its site of origin.
One of the most exciting emerging therapies in the treatment of cancer is targeted immunotherapya treatment that uses a person's immune system to fight cancer.
Immunotherapy harnesses the power of the body’s immune system to control the spread of cancer and attack the lurking cancer cellsthe basic structural and functional unit of all living things to eliminate them. Non-personalised immunotherapy generally activates a broad range of immune cells, thereby sometimes triggering severe auto-immune reactions. But if clinicians can use Next Generation Sequencing to reveal the genetic profile of tumours, more personalised immunotherapy agents can be used, based on the precise individual genetic, molecular and immune profile of that cancer. Sometimes, combining both strategies, called ‘precision immuno-oncology’ provides the best, most effective therapies. It’s certainly one of the most fast-paced, active areas in cancer research currently.
Some immunotherapies are also targeted therapies, which are directed to specific tumours and molecular alterations. Some of those are called checkpoint inhibitors, which use antibodies to stimulate the immune system against residing cancers. Instead of activating all the immune cells, immune checkpoint inhibitors work by interfering with the mechanism that cancer cells use to evade the host’s immune response. One type of immunotherapy, CAR-T is taking off in the battle against certain bloodthe red bodily fluid that transports oxygen and other nutrients around the body cancers by genetically modifying a person’s own T cells so that they recognise circulating cancer cells as foreign, thereby attacking and killing them. Learn more about CAR-T here.
The difference between these personalised medicine treatments and conventional treatments is stark – improved outcomes with fewer side effects:
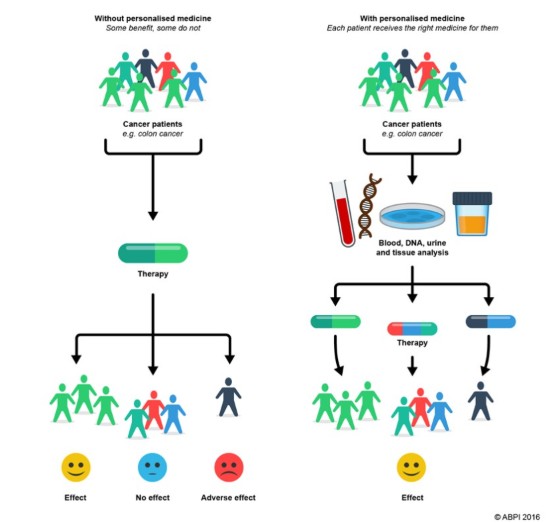
The following shows how people are screened for a targeted therapymedication that targets specific molecular features of cancer cells, and how they’re then monitored for response:
Thanks to evolving sequencing technologies, a whole range of new therapies are emerging in the cancer space – all of which are looking to greatly improve rates of early diagnoses, the efficacy of treatment, and long-term prognoses whilst reducing side effects during treatment.
If you’d like any further information about targeted therapies, please contact us at Rare Cancers Australia on 1800 257 600 or email [email protected].
